Focus on Broadband and Maternal Health
Access to reliable broadband connectivity is a critical tool for improving maternal and infant health outcomes across the United States. While maternal mortality rates have decreased (opens new window) in recent years, the prevalence of severe maternal morbidity has risen (opens new window) and in 2022, the infant mortality rate increased for the first time in two decades (opens new window). These troubling trends highlight the need for innovative solutions to address health disparities, particularly in rural communities (opens new window). Research suggests that many of these deaths, complications, and inequities can be prevented (opens new window).
The Key Role of Broadband Connectivity
Broadband connectivity has shown significant promise in improving maternal health outcomes, particularly in unserved and remote areas. For instance, meta-analyses have shown that digital health interventions reduce the risk of adverse outcomes for pregnant women with gestational diabetes (opens new window), improve infant health outcomes (opens new window), and reduce symptoms of depression and anxiety among women with post-partum depression (opens new window). These solutions leverage connectivity, mobile devices, and digital tools to provide timely information, access to care, and monitoring during pregnancy, childbirth, and postpartum periods. Below are examples of such technologies:
- Mobile health (mHealth) apps empower pregnant women with tools to track their baby’s development, monitor health symptoms, and access pregnancy-specific educational resources. These apps have been shown to improve outcomes, such as supporting successful breastfeeding (opens new window). Looking ahead, mHealth apps will likely leverage AI to provide personalized recommendations, predict potential risks, and encourage proactive care for healthier pregnancies.
- Broadband-powered AI chatbots offer pregnant women instant access to maternal health advice, answer questions, and provide guidance on pregnancy-related concerns. These conversational tools (opens new window) have been shown to improve health knowledge, encourage positive behaviors, and help prevent risks before and during pregnancy.
- Wearable devices, such as smartwatches and connected sensors, help pregnant women monitor vital signs like heart rate, blood sugar, and blood pressure from anywhere, making them especially valuable for those in remote areas. These tools can improve outcomes, such as reducing the risk of babies born with low oxygen levels (opens new window). In the future, pregnancy-specific wearables could track fetal movement, uterine contractions, and other important health metrics to support safer pregnancies.
- Telemedicine platforms allow pregnant women to connect with obstetricians, midwives, and other healthcare providers through video calls, phone, or chat. These remote consultations provide safe and effective care, offering outcomes comparable to in-person visits (opens new window) for high-risk pregnancies while improving convenience and accessibility.
- Virtual reality (opens new window) (VR) technology can help pregnant women manage anxiety, reduce pain, and stay active during pregnancy and childbirth. VR can also simulate the delivery process in a realistic, immersive environment, allowing women to experience and prepare for childbirth in advance, helping to ease fears and build confidence.
In the U.S., broadband and mobile technologies are transforming maternal health by improving access, education, and monitoring. Future advancements in AI, wearable devices, and virtual care could further enhance outcomes and reduce disparities, but reliable broadband is essential. For instance, faster internet speeds enable more frequent use of telehealth (opens new window) and remote monitoring (opens new window), while lack of connectivity limits access, especially in rural and tribal areas where 28% and 23% of residents (opens new window), respectively, lack adequate broadband. Addressing these gaps is critical to expanding connected health solutions in rural areas and for other vulnerable populations.
Background on Maternal Health in the United States
In addition to the increasing maternal morbidity and high maternal mortality rates:
- The U.S. is facing the increasing prevalence of worsening mental health and substance use disorders among reproductive-age and pregnant women. For example, the number of women with opioid-related diagnoses at delivery increased by 131% between 2010 and 2017 (opens new window). Mental health issues and substance use have been associated with poor maternal health outcomes.
- Women have also started having children later in life, with the mean age of mothers at first birth reaching a record high, at 30 years (opens new window). The risk of developing chronic conditions such as hypertension (opens new window) and gestational diabetes (opens new window) during pregnancy increases with age, leading to a higher likelihood of poor maternal health outcomes. Infants born to women with chronic conditions are also at a higher risk of experiencing poor outcomes (opens new window).
- Access to maternal health care remains a significant challenge, especially for women in rural areas and from lower income households. According to the March of Dimes (opens new window), more than 2.3 million women of childbearing age live in “maternity care deserts”—areas where there are no hospitals or birth centers offering obstetric care and no obstetric providers—and an additional 3 million women live in counties with limited access to maternity care.
- Recent data show that over 80% of maternal deaths could be prevented (opens new window). Telehealth and other broadband-enabled solutions and technologies can be a part of the toolkit for improving maternal health and addressing preventable deaths. Prior work by the Connect2HealthFCC Task Force (Task Force) has also shown that populations living in counties that have higher broadband connectivity tend to have better health (opens new window), strongly suggesting that access to and adoption of broadband itself may be related to improvements in health and health outcomes.
Mapping the Intersection of Broadband and Maternal Health
To address maternal health challenges, the FCC is playing an important role in advancing connected health and improving access to care through telehealth and broadband-enabled technologies. The Data Mapping to Save Moms’ Lives Act (Public Law No: 117-247 (opens new window)), enacted in December 2022, directed the FCC to integrate publicly available maternal health data into its Mapping Broadband Health in America platform, in consultation with the Centers for Disease Control and Prevention (CDC). This initiative aims to enhance maternal care quality and reduce poor health outcomes (opens new window) by identifying areas with high maternal health need and limited telehealth resources.
The platform was first updated in June 2023 to display the intersection of broadband connectivity and maternal health outcomes. Subsequent updates in December 2024 and 2025 added more maternal and infant health data and new features to support decision-making. Users can:
- Assess Internet connectivity in areas with high maternal mortality, severe maternal morbidity, or infant mortality.
- Generate insights to inform policies and programs that leverage broadband to improve maternal and infant health outcomes and address disparities.
- Create customized maps at state and county levels, displaying broadband connectivity (e.g., fixed and mobile access, Internet adoption rates, rural access) alongside maternal health data.
- Filter maternal health data by demographics, socioeconomic factors, maternal age, race/ethnicity, prenatal care, and rurality to identify potential areas for broadband-enabled interventions.
To meet the Data Mapping to Save Moms’ Lives Act’s requirements, the FCC Task Force implemented a multi-phase approach, consulting with the CDC, HHS agencies, and other stakeholders to determine which maternal health data to include. In October 2023, the Commission issued a Notice of Inquiry (opens new window) to gather public input on enhancing the platform’s capabilities. Additionally, the Task Force hosted a November 2023 roundtable, titled “The Connected Future of Maternity Care: Intersecting Maternal Health and Broadband Data,” bringing together experts to discuss broadband’s potential to improve maternal health outcomes. Using stakeholder feedback, the Task Force developed a conceptual framework to guide platform development, and the 2025 release includes an updated conceptual model (shown below) to outline the complex intersection of broadband and maternal health.
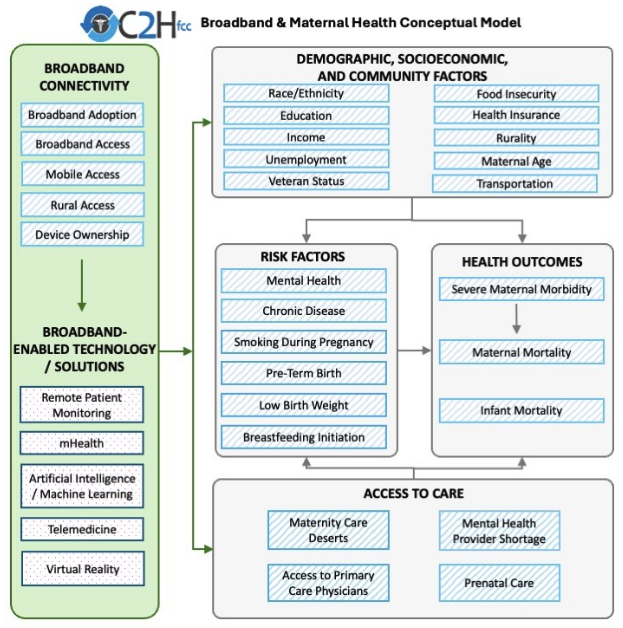
KEY: Blue diagonal lines denote items included in previous releases and pink dots represent technology solutions that use broadband connectivity and can improve maternal health outcomes (note that the platform does not include data for this set of variables).
The Task Force identified key broadband connectivity factors that enable the use of digital solutions to improve maternal health outcomes.
- Broadband Adoption: Based on 2019-2023 Census American Community Survey data, on average approximately 75% of households in a county report subscribing to high-speed Internet (e.g., cable, DSL, fiber optic).
- Fixed Broadband Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average approximately 92% of individuals in a county have access to fixed terrestrial broadband service at 100/20 Mbps or higher advertised speeds.
- Mobile Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average around 97% of individuals in a county have access to outdoor stationary mobile 5G-NR service at 35/3 Mbps or higher advertised speeds.
- Rural Fixed Broadband Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average around 90% of those living in rural census blocks have access to fixed terrestrial broadband service at 100/20 Mbps or higher advertised speeds.
- Device Ownership: Based on 2019-2023 Census American Community Survey data, on average approximately 6% of households in a county report having no computing devices. Access to digital devices (opens new window) is associated with preferring telehealth appointments over in-person visits.
- Funding: The FCC's Rural Health Care Program provides funding to eligible healthcare providers for telecommunications and broadband services necessary for the provision of health care. Over 2900 counties have received some level of funding between 2019 and 2024.
The Task Force identified relevant maternal health outcomes where broadband-enabled interventions might help bridge the gaps. The HEALTH OUTCOMES box of the framework includes three measures on the platform.
- Severe Maternal Morbidity: Not all women who suffer serious and life-threatening complications of pregnancy die from these causes. Instead, many experience “unexpected outcomes of labor and delivery (opens new window) that result in significant short- or long-term consequences,” called severe maternal morbidity. These “near-misses” for maternal death include 20 severe indicators (opens new window) that women can experience during delivery hospitalization, like hysterectomy, ventilation or temporary tracheostomy.
- Maternal Mortality Rate: The World Health Organization defines maternal mortality as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy (opens new window), from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.”
- Infant Mortality Rate: The CDC defines infant mortality as “number of deaths under age 1 year per 1,000 live births (opens new window).” Key factors that influence maternal health outcomes, such as access to prenatal care and chronic disease, also impact infant health outcomes including infant mortality.
Much of the data for severe maternal morbidity and maternal mortality outcomes are either unreliable or suppressed (opens new window) at the county level due to low numbers, meaning that those data are only available at the state level. The need for more reliable data on maternal health at the county level has previously been noted in the Surgeon General’s Call to Action to Improve Maternal Health (opens new window). The Task Force uses risk factors such as hypertension, gestational diabetes, and obesity as proxy variables, given their availability at the county level and their association with severe maternal morbidity and maternal mortality outcomes.
The Task Force identified relevant demographic factors that influence maternal health outcomes and where broadband-enabled interventions might help bridge the gaps. The DEMOGRAPHICS, SOCIOECONOMIC, AND COMMUNITY FACTORS box of the framework includes: maternal age, race & ethnicity, education*, income*, unemployment*, Veteran status, food insecurity*, health insurance*, transportation*, and rurality*.
The Task Force also identified relevant risk factors that influence maternal health outcomes and where broadband-enabled interventions might help bridge the gaps. The RISK FACTORS box of the framework includes six measures:
- Mental Health*: Depression affects 1 in 10 women (opens new window) aged 18-44 years of age. Mental health conditions, including suicide, overdose/poisoning related to substance use disorder, are the leading cause (opens new window) of pregnancy-related death.
- Chronic Disease: Chronic conditions like obesity (opens new window), hypertension (opens new window), and gestational diabetes (opens new window) can increase the likelihood of poor maternal and infant health outcomes. Maternal obesity is linked (opens new window) to gestational diabetes, hypertension, preeclampsia, preterm delivery, and infant death. Hypertension is one of the most common pregnancy complications and a leading cause of pregnancy-related death with higher rates of Black women and American Indian Alaskan Native women as well as women over 35.
- Smoking during Pregnancy: Smoking during pregnancy can lead (opens new window) to low birth weight, pre-term birth, stillbirth, birth defects, sudden infant death syndrome (SIDS) and abnormal maternal bleeding. It can also cause fertility problems for future pregnancies.
- Veteran Prevalence*: Pregnant Veterans are more likely (opens new window) to have poor maternal health and mental outcomes in comparison to civilian women. Military service (opens new window) adds unique risks, including sexual trauma, injuries, mental health issues, and environmental exposures, further increasing the risk of poor pregnancy outcomes, like preterm birth.
- Pre-Term Birth: Pre-term birth affects approximately 1 in 10 infants (opens new window) in the United States and is a leading cause of infant mortality. Women over 35, those with lower incomes, and Black, Native Hawaiian, Pacific Islander, American Indian, or Alaska Native women face a higher risk of pre-term birth.
- Breastfeeding Initiation: For infants, breastfeeding is associated (opens new window) with lower rates of asthma, diabetes, obesity, cancer, and SIDS. For mothers, breastfeeding is associated (opens new window) with lower risk of Type 2 diabetes, breast, and ovarian cancer. Breastfeeding rates are lower (opens new window) for Black, Native Hawaiian, Pacific Islander, American Indian, or Alaska Native women. There are also significant connections (opens new window) between breastfeeding and maternal mental health outcomes.
The Task Force identified relevant access to care components that influence maternal health outcomes and where broadband-enabled interventions might help bridge the gaps. The ACCESS TO CARE box of the framework includes four measures:
- Maternity Care Deserts: Areas with little to no maternal care resources (opens new window), which may also have lower access to broadband services. Some researchers estimate that 70% of counties (opens new window) with the highest proportion of low-speed Internet providers did not have full access to maternity care.
- Mental Health Provider Shortage Areas*: Areas with limited mental health providers and resources. Maternal mental health conditions affect 1 in 5 women (opens new window) during or after pregnancy and are one of the most common causes of pregnancy-related deaths (22.7%) (opens new window). Broadband connection can enable digital capabilities such as navigating care, identifying risks, building community, and connecting to counseling as needed. Telehealth services can help connect patients and mental health providers (opens new window).
- Access to Primary Care Providers*: Primary care providers often serve as obstetric providers (opens new window), especially in rural areas, before, during, and after pregnancy. This is due to an obstetric care workforce shortage across the country.
- Prenatal Care: Babies without prenatal care are three times (opens new window) more likely to have a low birth weight and five times more likely to experience infant mortality.
Information on the data sources can be found on the Data page.
*The data on these variables pertain to the general population and do not specifically focus on pregnant or postpartum individuals.
Future Work
The Mapping Broadband Health in America platform is a foundational tool for understanding the intersection of broadband and health, giving policymakers, researchers, advocacy groups, broadband service providers, innovators, and other interested parties a concrete path to a more connected and healthier future for all Americans.
The Task Force will continue to refine the conceptual approach going forward and welcomes comments and suggestions from interested parties via e-mail to engageC2H@fcc.gov(opens new browser window with "Mapping" in the subject line).