Focus on Broadband and Opioids
The opioid crisis deeply impacts communities and families across the United States. The opioid epidemic was officially declared a public health emergency in 2017 under section 319 of the Public Health Service Act. This declaration has been consistently renewed, with the most recent renewal occurring in March 2025 (opens new window). Tragically, this crisis claims the lives of more than 224 Americans every day (opens new window).
The Key Role of Broadband Connectivity
Broadband technology can play an important role in the fight against the opioid crisis, with the potential to save and improve lives across the United States.
- Telehealth services for behavioral health and substance use disorder treatment. Telehealth services, powered by reliable broadband access, have been shown to enhance access to and delivery of behavioral health care (opens new window), including treatment for substance use disorders. Recent research highlights promising outcomes: The use of telehealth services and medications for Opioid Use Disorder (OUD) is associated with reduced (opens new window) risk of fatal overdoses. Additionally, telehealth has been linked to an increased likelihood of individuals staying in treatment for OUD (opens new window). Via telehealth, individuals in rural or unserved areas can connect with healthcare providers, addiction specialists, and counselors without needing to travel long distances.
- Crisis hotlines for immediate support. Crisis hotlines, including the Substance Abuse and Mental Health Services Administration (SAMHSA)’s helpline (opens new window) and text messaging service (opens new window), are accessible via broadband or mobile connections to provide immediate assistance. These services offer referrals to local treatment facilities, support groups, and community-based organizations, ensuring individuals receive the help they need. In 2020 alone, the SAMSHA Helpline received 833,598 calls (opens new window), underscoring the vital role these resources play in supporting individuals and communities.
- Employment and housing resources for individuals in recovery. Broadband access plays a critical role in connecting individuals in recovery to essential resources such as job opportunities, housing assistance, and other support services. Employment (opens new window) not only helps individuals recovering from opioid use disorder (OUD) afford health insurance and treatment but also reduces social isolation and lowers the risk of homelessness or suicide. Stable housing (opens new window) is equally vital, as a lack of housing increases vulnerability to risky substance use, mental health challenges, and recurrence of substance use disorders. Research shows that broadband availability is associated with lower unemployment rates, including in rural areas (opens new window).
- Digital health interventions for treatment. Digital health interventions that complement in-person drug treatment have been shown to reduce (opens new window) the risk of relapse and decrease days of opioid use. These tools include prescription digital therapeutic applications for mobile phones that provide cognitive behavioral therapy to improve retention in outpatient opioid use disorder (OUD) treatment, as well as apps that support transitional care for addiction and co-occurring mental health disorders. Other digital (mobile phone) applications focus on opioid overdose education and emergency response, assist with cravings and relapse prevention during recovery, or guide patients through medication-assisted therapy.
- Digital interventions for pain management. Digital interventions for pain management (opens new window) can support individuals with OUD by reducing reliance on medical opioids and addressing opioid misuse behaviors. These tools enable users to log pain levels, identify triggers, and track patterns to better understand factors that worsen or alleviate pain. They also assist individuals in setting realistic goals and monitoring progress over time. Some digital interventions integrate wearable devices to teach biofeedback techniques, allowing users to regulate physiological responses such as heart rate and muscle tension to manage pain effectively. Virtual-reality interventions offer immersive experiences that can distract from pain, reduce anxiety, and promote relaxation. Additionally, apps may provide physical therapy guidance, including tailored exercises, stretches, and movement programs designed to address chronic pain conditions. These tools can be particularly helpful for Veterans (opens new window), as musculoskeletal pain is the most prevalent health condition.
These examples underscore the critical role that broadband-enabled solutions can play in addressing this urgent public health challenge. These innovative digital solutions expand access to critical resources and enhance treatment outcomes.
Background on Opioid Misuse in the United States
Opioid drugs (opens new window) include prescription medications to treat pain and illegal drugs like heroin. Opioids are addictive, and their use—either by themselves or in combination with other drugs—is a major driver of the drug overdose crisis in the United States. The Centers for Disease Control and Prevention (CDC) characterizes the opioid crisis in three distinct waves (opens new window) identified by the primary type of opioid driving the spike in overdose and mortality.
- Wave 1 (1990s): The crisis began in the 1990s with a first wave of deaths due to a rise in overdoses involving prescription opioids, including natural and semi-synthetic opioids and methadone.
- Wave 2 (2010 - 2013): This was followed by a second wave in 2010 with a spike in heroin-involved deaths.
- Wave 3 (2013 - present): The present wave is defined by a rapid increase in deaths due to synthetic opioids other than methadone (opens new window) (including fentanyl, fentanyl analogs, and tramadol) since 2013. Between 2021 and 2022, synthetic opioid deaths increased by 4% (opens new window) and now account for about 90% of opioid-involved deaths.
According to the CDC:
- Nearly 727,000 people (opens new window) in the United States have died from overdoses involving opioids since the epidemic began;
- The number of annual opioid overdose deaths remains more than six times higher (opens new window) than it was in 1999;
- There were approximately 105,007 opioid overdose deaths in 2023 (opens new window) and 72,776 involved synthetic opioids other than methadone (opens new window); and
- Provisional data reflects that the number of drug overdose deaths began to decrease in 2023 (opens new window), the first time since 2018, and continued to decline in 2024 (opens new window), although much work remains.
Of course, opioid overdoses may also be non-fatal. These non-fatal opioid overdoses place significant burdens on governments, health systems, communities, and families and may disproportionally affect rural and underserved areas. For example:
- There were 131,620 nonfatal opioid overdose emergency department visits and 54,044 inpatient hospitalizations (opens new window) in 2023,
- Most of these hospitalizations and emergency visits were paid for by Medicare, Medicaid, or the uninsured (opens new window).
- Rural counties may experience resource shortages or limited economic opportunities that negatively affect access to health care services and health outcomes.
Mapping the Intersection of Broadband and Drug Misuse
In recognition of the potential of broadband to help stakeholders respond to this crisis, particularly in rural areas, Congress (opens new window) directed the Federal Communications Commission (FCC) to update its Mapping Broadband Health in America platform to include data on drug misuse. In response, the Connect2HealthFCC Task Force launched a novel analytic and consultative process to determine how best to intersect broadband and drug misuse data in ways that would draw meaning from the data and lead to actionable intelligence for policymakers and other stakeholders. For instance, policymakers can examine which counties have both low internet adoption and high OUD prevalence along with shortages in mental health services to identify areas that could benefit from increased access to telemental health services. We used an evidence-based approach to conceptualize the intersection between drug and opioid misuse and connectivity, with a particular focus on identifying areas where broadband-enabled interventions could make a difference in access to care or health outcomes.
Multi-phase effort
The integration of drug misuse data into the Mapping Broadband Health in America platform is a multi-phase project and the most recent refinements reflect thoughtful review of the broadband and opioid landscape, as well as input and feedback from key stakeholders and users.
In the December 2024 release, a number of new variables relevant to the broadband connectivity and opioid misuse relationship were added, including digital device ownership, updated broadband access and adoption variables, access to care via transportation, poor mental health days, health insurance coverage by type (e.g., private, Medicaid, Medicare), OUD prevalence, Veteran prevalence, race and ethnicity, food insecurity, social vulnerability, and HIV prevalence.
The platform - which is available via www.fcc.gov/health/maps (opens new window) - allows users to identify and characterize the specific broadband/opioid challenges at the local level, point to solutions, and spark collaborations. Specifically:
- Users can ask questions like, what is the status of Internet connectivity in areas where the opioid crisis is being driven by higher prescription rates (i.e., there may be a need to augment prescription drug monitoring programs and connectivity for health) versus illicit drug use.
- Users can display selected data on opioid mortality and prescription rates from the CDC with the fixed broadband deployment data from the FCC to generate customized national, state, and county maps to explore the intersection between drug misuse and Internet connectivity. In addition to fixed broadband access, the platform visualizes metrics on Internet adoption, rural broadband access, and device ownership in a selected geographic area.
- Percent change in opioid mortality and prescription rates enable users to visualize trends and identify potential emerging “hotspots” of the crisis, where broadband-enabled interventions might prove fruitful.
- Opioid mortality rates and trends are broken down into several categories that reflect shifts in the primary type of opioid driving the crisis as it has evolved.
- Risk factors affecting opioid misuse and overdose have been added, including poor mental health days and access to healthcare (such as transportation, mental health provider shortages, and health insurance coverage).
- Opioid Use Disorder prevalence, a key health outcome variable, has been added.
- Users can also filter by rurality and overlay other key community factors (such as race and ethnicity, and veteran status), and important economic indicators (including poverty and the unemployment) to better understand the intersection between drug misuse and broadband.
- One ongoing challenge is the reality that community-level data are not available for all relevant data points; we hope to further tackle those pre-existing data gaps in later refinements.
To determine how best to intersect connectivity and opioids data, the Task Force began by reviewing the available literature on opioids and connected health. The goal was to inform a conceptual model for intersecting broadband and drug misuse data. Specifically, we identified key evidence-based factors that were important to better understand and address opioid use disorder, overdose, and mortality at a population level – forming a potential roadmap for leveraging broadband, telehealth, and other advanced broadband-enabled health technologies as part of the overall solution. These factors and their relationships are presented in the resulting Conceptual Model that underlies the current mapping platform.
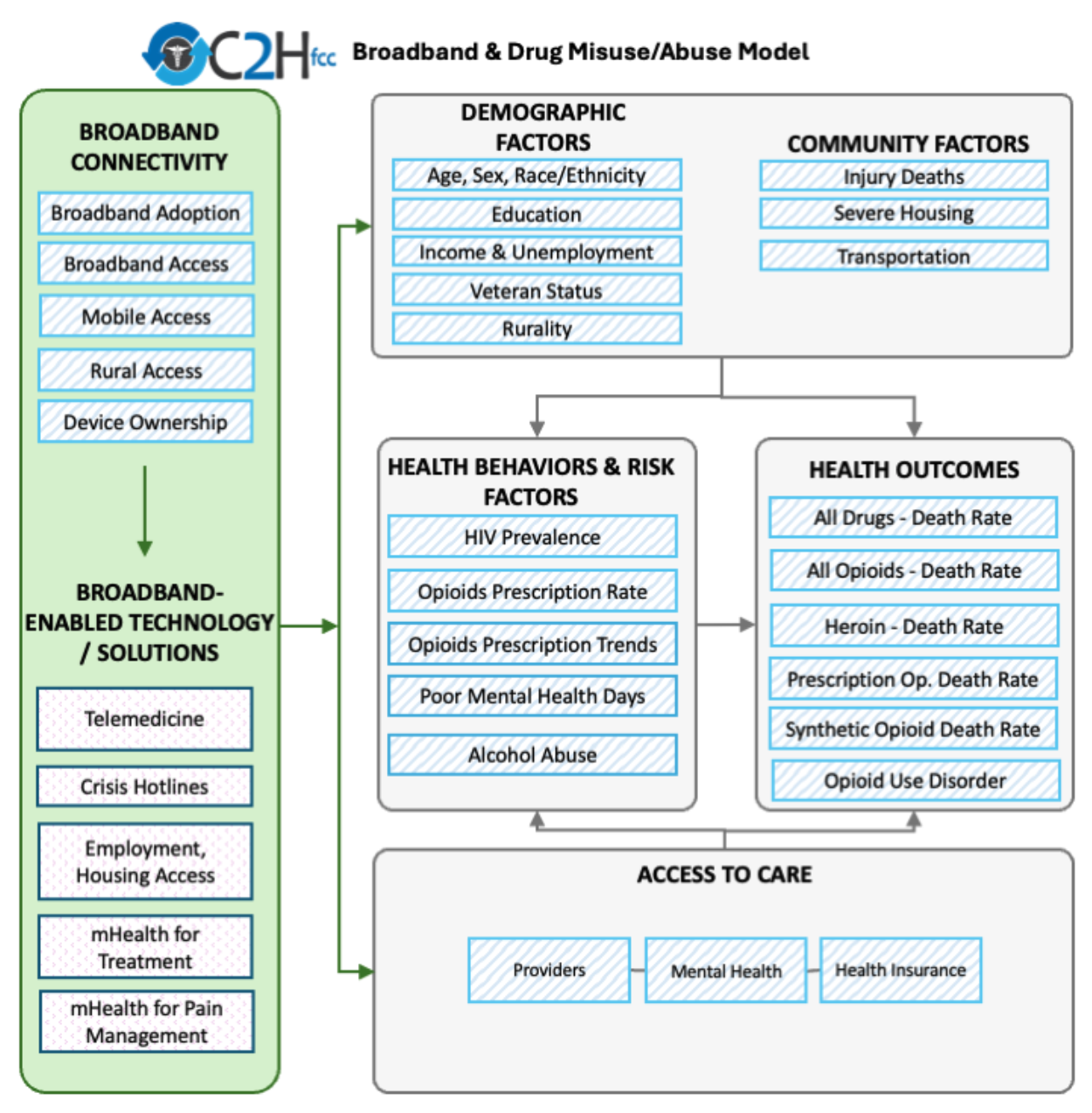
KEY: Blue diagonal lines denote items included in previous releases; and pink dots represent technology solutions that use broadband connectivity and can improve chronic disease outcomes (note that the platform does not include data for this set of variables).
The Task Force identified key broadband connectivity factors that enable the use of digital solutions to address opioid misuse outcomes.
- Broadband Adoption: Based on 2019-2023 Census American Community Survey data, on average approximately 75% of households in a county report subscribing to high-speed Internet (e.g., cable, DSL, fiber optic).
- Fixed Broadband Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average approximately 92% of individuals in a county have access to fixed terrestrial broadband service at 100/20 Mbps or higher advertised speeds.
- Mobile Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average around 97% of individuals in a county have access to outdoor stationary mobile 5G-NR service at 35/3 Mbps or higher advertised speeds.
- Rural Fixed Broadband Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average around 90% of those living in rural census blocks have access to fixed terrestrial broadband service at 100/20 Mbps or higher advertised speeds.
- Device Ownership: Based on 2019-2023 Census American Community Survey data, on average approximately 6% of households in a county report having no computing devices. Access to digital devices (opens new window) is associated with preferring telehealth appointments over in-person visits.
- Funding: The FCC's Rural Health Care Program provides funding to eligible healthcare providers for telecommunications and broadband services necessary for the provision of health care. Over 2900 counties have received some level of funding between 2019 and 2024.
The Task Force identified relevant opioids outcomes where broadband-enabled interventions might help bridge the gaps. The HEALTH OUTCOMES box of the framework includes six measures on the platform.
- All drugs: Deaths and trends due to all drug overdoses for any reason (unintentional, suicide, homicide, or undetermined). Drug overdose deaths are a national public health emergency (opens new window).
- Any opioid: Deaths and trends due to overdoses for any reasons and involving opium, heroin, natural and semi-synthetic opioids, methadone, synthetic opioids other than methadone, and other and unspecified narcotics. The majority (opens new window) of drug overdose deaths involve opioids.
- Heroin: Deaths and trends due to overdoses for any reason and involving heroin. While the number of overdose deaths due to heroin alone has decreased since 2016, the proportion of overdose deaths co-involving heroin and illicitly manufactured fentanyl (opens new window) has increased significantly in 2022 and 2023.
- Prescription opioids: Deaths and trends due to overdoses for any reason and involving natural and semi-synthetic opioids and methadone. Commonly prescribed opioids, though a key cause of drug overdose deaths from 1999 to 2017 (opens new window), are no longer the main driver of drug overdoses.
- Synthetic opioids: Deaths and trends due to overdoses for any reason and involving synthetic opioids other than methadone. Since 2017, synthetic opioids (opens new window) other than methadone have become the leading driver of drug overdose deaths.
- Opioid use disorder: Prevalence of overarching Opioid Use Disorder (OUD) among Medicare (dual and non-dual) beneficiaries. Between six and eight million adults (opens new window) in the U.S. are currently living with OUD.
The Task Force identified relevant demographic factors that influence opioid misuse outcomes and where broadband-enabled interventions might help bridge the gaps. The DEMOGRAPHICS, SOCIOECONOMIC, AND COMMUNITY FACTORS box of the framework includes eleven measures:
- Age: Young and middle-aged adults (opens new window) are primarily affected by opioid use disorder.
- Sex: Males (opens new window) are at higher risk of opioid use disorder.
- Race/ethnicity: White race is associated with a higher risk for opioid use disorder (opens new window), though non-Hispanic Black individuals have had greater increase (opens new window) in opioid overdose-related mortality than other groups in recent years.
- Education: Lower educational attainment (opens new window) is associated with higher risk of opioid use disorder.
- Income: Lower income (opens new window) is associated with higher risk of opioid use disorder.
- Unemployment: Unemployment (opens new window) is associated with higher risk of opioid use disorder.
- Veteran status: Prescription opioid misuse (opens new window) is prevalent among veterans.
- Rurality: The Opioid epidemic significantly impacts rural communities (opens new window) where mortality rates due to misuse have at times surpassed urban communities.
- Injury deaths: Opioid overdoses are leading cause of injury deaths (opens new window) in the United States.
- Severe housing: Stable housing (opens new window) is vital for opioid misuse recovery, as a lack of housing increases vulnerability to risky substance use, mental health challenges, and recurrence of substance use disorders.
- Transportation: Lack of transportation (opens new window) has been identified as a barrier to opioid use disorder treatment.
The Task Force also identified relevant risk factors that influence opioids misuse outcomes and where broadband-enabled interventions might help bridge the gaps. The RISK FACTORS box of the framework includes four measures:
- HIV prevalence: Chronic pain is more common among HIV-infected individuals (opens new window), who receive higher doses of opioids and are more likely to have a substance use disorder, mental illness, and opioid misuse.
- Opioid prescription (Rx) rates and trends provide information on the number of prescriptions in a community that may indicate availability and exposure to opioids.
- Poor mental health days reflect the burden of disabilities and chronic diseases as well as health-related quality of life among individuals living in a community. People with untreated psychiatric disorders or psychiatric comorbidities are at increased risk (opens new window) for opioid misuse and mortality.
- Alcohol and other substance misuse may create an environment that enables opioid misuse and overdose. People with a history of substance use disorders (opens new window) are at higher risk of OUD.
The Task Force identified relevant access to care components that influence opioids misuse outcomes and where broadband-enabled interventions might help bridge the gaps. The ACCESS TO CARE box of the framework includes three measures:
- Access to healthcare providers: Higher density of primary care clinicians (opens new window) is associated with lower risk of opioid overdose and higher likelihood of having capacity to deliver medications to treat OUD.
- Access to mental health providers: provides information on the availability of services for individuals to both seek preventive care and receive treatment for opioid misuse.
- Health insurance: Lack of health insurance (opens new window) is a key barrier to opioid use disorder treatment.
Information on the data sources can be found on the Data page.
Future Work
The Mapping Broadband Health in America platform is a foundational tool for understanding the intersection of broadband and health, giving policymakers, researchers, advocacy groups, broadband service providers, innovators, and other interested parties a concrete path to a more connected and healthier future for all Americans.
The Task Force will continue to refine the conceptual approach going forward and welcomes comments and suggestions from interested parties via e-mail to engageC2H@fcc.gov(opens new browser window with "Mapping" in the subject line).